The cornea is the outermost layer of the eye and is the clear tissue that covers the colored iris and pupil. Its role is to focus light through its high powered refractive surface and protect the inner-workings of the eye. It contains no blood to protect it against infection. If it is injured or affected by disease, it may become swollen or scarred, and its smoothness and clarity may be lost. Scars, swelling or an irregular shape can cause the cornea to scatter or distort light, resulting in glare, blurry vision, or even pain.
Abrasions and injuries to the cornea can be very painful; causing blurred vision, tearing and sensitivity to light. The good news is that minor abrasions of the cornea, although very painful, heal quickly. But the worry is that deeper abrasions can cause scarring, resulting in vision impairment, and in some cases, a need for corneal transplant.
There are many conditions that can affect the clarity of the cornea. For instance, injury to the cornea can cause scarring as can infections (especially herpes keratitis and conjunctivitis). Shingles of the head and neck often travel to the eye (anchor), affecting the cornea. A hereditary condition called Fuchs’ Dystrophy(anchor) causes corneal failure and Keratoconus(anchor) causes a steep curving of the cornea. Pterygiums sometimes impair vision and need to be removed. Dry Eye Disease (link out) is a common corneal condition that we treat every day. And sometimes corneal failure can also occur after an eye surgery. These are a few of the most common corneal conditions that we treat here at The Eye Associates. Some of the treatment options include corneal transplants, treatments with amniotic membrane tissues, drops, and even contact lenses.
Fuchs’ Dystrophy is a corneal disease that reduces the number of cells that make up the inner layer of the cornea. A typical characteristic of Fuchs’ is dewdrop-shaped outgrowths, called guttata, in the layer just underneath the endothelial cell layer. These growths can scatter light and significantly interfere with vision, much like what happens with a cataract
Fuchs’ Dystrophy is a progressive corneal disease and because of this, over time, changes to the corneal cells may interfere with vision. If guttata or corneal swelling are causing a significant decrease in vision, surgery may be necessary to remove the scar tissue.
Fuchs’ Dystrophy is more common in women and is often seen in the 50s or 60s, although it can appear earlier in adulthood. We find a genetic component but it can also occur in individuals without a family history due to sporadic mutation. Those who inherited the condition from a parent have a 50 percent chance of passing it on to their children.
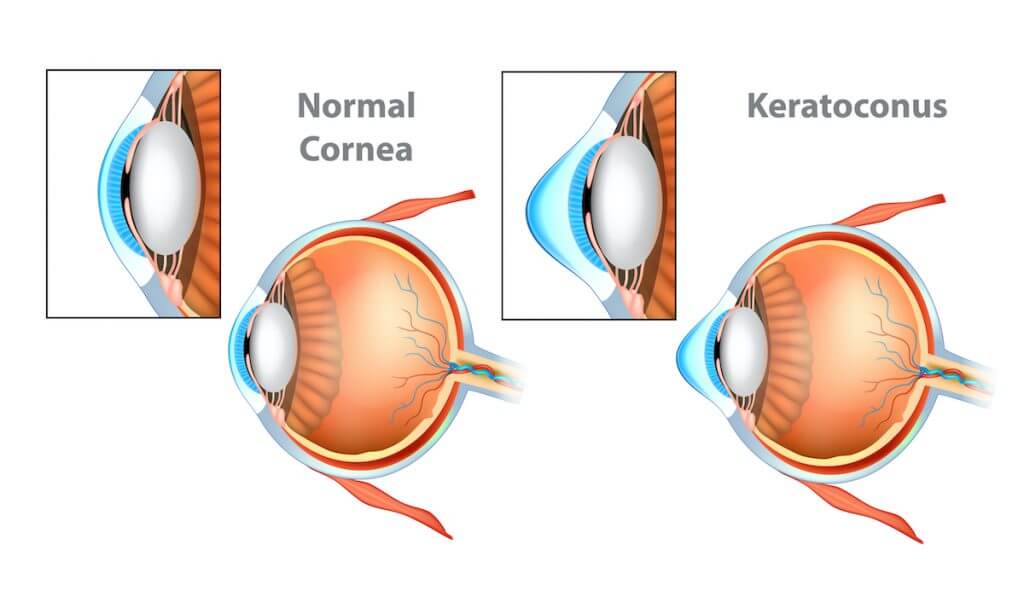
Keratoconus is a condition in which the normally round, dome-like cornea (the clear front window of the eye) becomes thin and develops a cone-like bulge. Keratoconus literally means “cone-shaped cornea”. When the shape of the cornea is altered by the disease, vision is distorted, making activities like driving, typing on a computer, watching television or reading difficult.
Keratoconus appears to run in some families but it has also been associated with excessive eye rubbing and prolonged contact lens wear. It also seems to occur more often with people with certain eye diseases, such as retinitis pigmentosa, retinopathy of prematurity and vernal keratoconjunctivitis as well as systemic diseases such as Leber’s Congenital Amaurosis, Ehlers-Danlos Syndrome, and Down Syndrome.
In the early stages, the patient will notice some slight distortion and sensitivity to light. Often these symptoms will show up in the teens through the early twenties. Even though keratoconus tends to progress slowly, it is a lifetime disease. As it gets worse, the most common complaints are increased astigmatism and/or near-sightedness, blurred vision, and frequent eyeglass prescription changes. Early stage patients with it can sometimes wear glasses, but as the condition progresses most patients need to wear specialized contact lenses in order to see their best. At The Eye Associates, our doctors are skilled at fitting the latest in contact lens treatments for this condition. Some of the options include rigid gas permeable (RGP) contact lenses, ‘piggybacking’ contact lenses, hybrid contact lenses, as well as scleral and semi-scleral contact lenses.
The Eye Associates that specialize in contact lens fittings for keratoconus patients. When good vision is no longer possible with contact lenses, a corneal transplant may be recommended. With this procedure, the surgeon removes the diseased portion of the cornea and replaces it with healthy donor tissue. He performs a revolutionary partial thickness transplant for keratoconus called Deep Anterior Lamellar Keratoplasty (DALK).
Pinguecula and Pterygium are often mistaken as being the same condition because they are both growths on the cornea and the conjunctiva. Both are common, especially here in Florida, and are non-cancerous. They may occur on one or both eyes. The exact cause is not known but it is thought that extended exposure to sun and eye irritation could contribute. That is one reason we always recommend wearing sunglasses with UV protection, especially for people with occupations and hobbies outdoors.
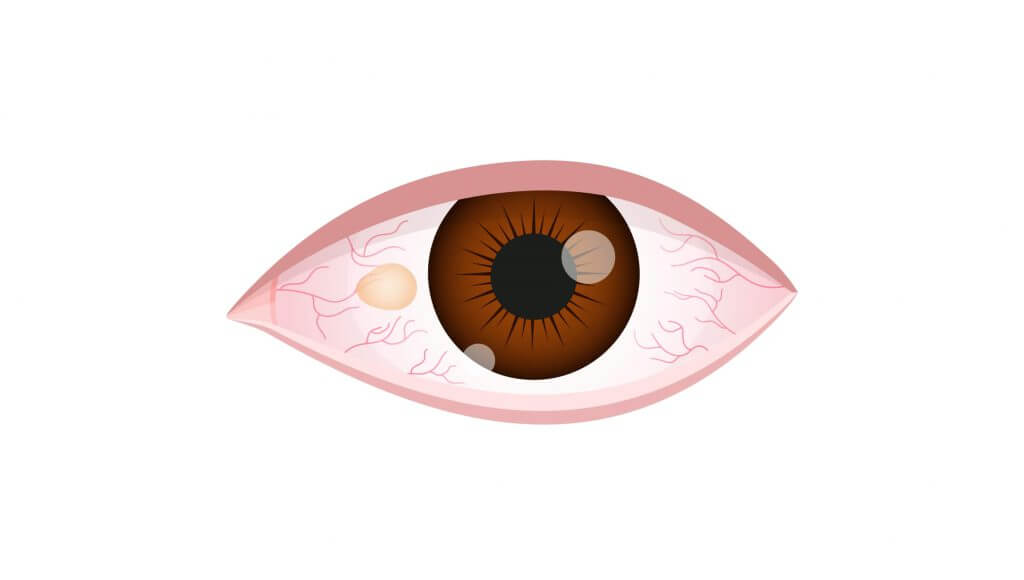

The difference between the two conditions is as follows: A pinguecula (pronounced pin- GWEK-yoo-la) is a yellowish, slightly raised bump on the conjunctiva (the thin membrane that covers the white part of your eye near the cornea). When a pinguecula grows larger over the cornea, it can lead to the formation of a pterygium (pronounced tur-IJ-ee-um), but a pterygium can develop on its own without the start of a pinguecula. A pterygium is triangular in shape, elevated, and the problem occurs when it grows over the cornea and causes scar tissue. Some grow quickly while others never grow at all.
Most pterygium and pinguecula don’t bother patients or require treatment. But if you have a burning sensation or the sensation of something being in the eye, there are treatments available. Artificial tears, nonsteroidal anti-inflammatory drugs, and steroid drops are tried first. If they don’t help, then surgery can also be used to remove the growth for functional as well as cosmetic reasons. Amniotic membrane grafts are often used to promote healing after surgery, offering minimal discomfort and scarring.
Just like you’ve heard again and again on those TV commercials…..It is caused by the varicella zoster virus, the same virus that causes chicken pox. Anyone who has had chickenpox is at risk for developing it.
Often it will start with a ‘feeling’…. a subtle burning, swelling, itching or tingling on only one side of the body. It is hard to diagnose at that point, especially if it is in the eye. Once the rash of fluid filled blisters appear, it is easy to confirm the condition. Shingles can be anyplace on the body but the most common area is the torso around the waist, and the second most common is the face and eye. Often we will see the first blister on the tip of the nose
Over a million US citizens will get it, and 10 to 20% of them will get it in or around the eye. The skin lesions it causes are very painful, but when you develop shingles in the eye, called herpes zoster ophthalmicus, you are at risk for vision loss.
Unlike most conditions, shingles can affect every part of the eye. We often see corneal abrasions, ulcers, inflammation of the cornea, glaucoma induced by shingles, and even retinal damage in patients with shingles. The good news is that if we see the patient in the early days of the outbreak, we can successfully treat it. Only rarely do we see patients with permanent vision loss.
As we age, our immune system gets weaker and can also be compromised by medications, illnesses, and stress. These things cause an increased risk for developing it. It is estimated that 1 in 3 Americans will get shingles at some point in their lifetime. It is also more prevalent in women.
Prevention is always the best treatment. We recommend that our patients 60 and older get the vaccine. While the vaccine does not ‘prevent’ shingles, it may lessen the severity of the episode.
If you develop it, it is important to seek treatment as soon as possible. At The Eye Associates, we will put a shingle patient in an ‘emergency’ spot so that they can be seen quickly.
And of course, you must take all medications as prescribed. It is nothing to mess around with.
Even though shingles can be shocking to look at, it is not contagious. But there have been cases when a child that has never had chickenpox comes into contact with an open lesion, then the child will develop chickenpox; not shingles.
It doesn’t always reoccur, but unfortunately it can. It mostly happens if you have a weak immune system or if you take medications that suppress your immune system. Also, it can even reoccur if you have had the vaccine. There are no guarantees.